The Centers for Medicare & Medicaid Services (CMS) included a proposal to create a new mandatory alternative payment model, the Transforming Episode Accountability Model (TEAM), in the fiscal year 2025 hospital inpatient prospective payment system (IPPS) proposed rule.
The CMS proposes to mandate participation of all IPPS hospitals in selected core based statistical areas (CBSAs). The CMS proposes to randomly select 25% of 803 eligible CBSAs.
The CMS proposes to test the mandatory TEAM model for five years, beginning Jan. 1, 2026, and ending Dec. 31, 2030. Hospitals would be required to participate in all five surgical episodes and would be the episode initiators and bear financial risk if the model is finalized as proposed.
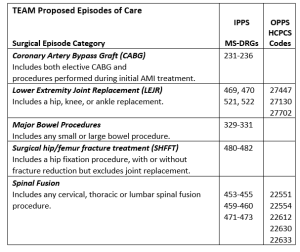
The model proposed to include five surgical episode categories for Medicare fee-for-service (FFS) beneficiaries:
An episode would begin with a Medicare FFS beneficiary’s acute care hospital stay or a hospital outpatient procedure visit. The episode would end 30 days after hospital discharge and would include the surgical procedure and inpatient stay, and all related care covered under Medicare Parts A and B within 30 days of discharge. The episode would exclude unrelated services.
The CMS would evaluate hospitals by comparing a participating hospitals’ actual Medicare FFS spending to their target price. The CMS would also evaluate performance on quality measures:
- Hospital readmission
- Patient Safety
- Patient-reported outcomes
The proposed model would not include Medicare Advantage plans, which currently cover 59% of Michigan Medicare beneficiaries. The CMS will accept comments until June 10 and anticipates release of a final rule Fall 2024.
Members with questions should contact Vickie Kunz at the MHA.