Improving Care in Michigan’s Rural Communities
I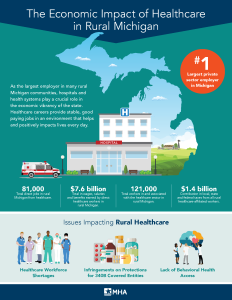 n Michigan’s rural communities, hospitals provide vital access to healthcare services, improving the health status of residents who may otherwise forgo care due to transportation challenges. These hospitals face unique funding challenges that can threaten the care and services they provide.
n Michigan’s rural communities, hospitals provide vital access to healthcare services, improving the health status of residents who may otherwise forgo care due to transportation challenges. These hospitals face unique funding challenges that can threaten the care and services they provide.
Rural Development Office
In January 2022, Governor Gretchen Whitmer signed a new executive directive establishing the Office of Rural Development. The new office is located within the Michigan Department of Agriculture and Rural Development advises organizations on how to best help rural areas. The key areas of focus for the Office of Rural Development are:
- Economic development
- Affordable housing
- Green energy
- Education
- Population changes
- High-speed internet
- Tribal issues
In addition, Governor Whitmer convened a roundtable to explore the most pressing issues the Office of Rural Development should periodize. Key stakeholders from across the state attended the roundtable, including MHA member David Jahn, the President and CEO of War Memorial Hospital.
The Michigan Department of Agriculture and Rural Development announced on March 15 the selection of Sarah Lucas as the new Deputy Director the Office of Rural Development. Ms. Lucas will start in her new role on April 18th and will be tasked with reinvigoration Michigan’s rural economics.
The MHA engages with the Office of Rural Development on efforts to support and advance rural health, and small and rural hospital needs. MHA members with questions should contact Lauren LaPine.
High-Speed Internet Access
Expanding access to high-speed internet access across the state of Michigan is a priority for both the Whitmer Administration and the MHA. In October 2020 Governor Whitmer announced the formation of the Connecting Michigan Taskforce, an interagency working group that aims to streamline efforts across state agencies and departments related to high-speed internet access. The Michigan High-Speed Internet Office, located within the Michigan Department of Labor and Economic Opportunity serves as the organizing body for addressing high-speed internet access.
The recently released Michigan Broadband Roadmap details the need for widespread access and highlights the areas across our state with the most severe access gaps. The MHA recognizes that access to high-speed internet is imperative in making telehealth and telemedicine possible, especially in rural communities. The MHA is working closely with the Michigan Legislature to advocate for funding to expand high-speed internet access and build the necessary infrastructure across our state.
At the federal level, the MHA advocates in support of the Telehealth Extension and Evaluation Act of 2021 (Sen. Cortez Masto (NV), Sen. Young (IN)) Prior to the COVID-19 pandemic, coverage of Medicare Part B services delivered via telehealth was generally limited to a subset of codes for patients in rural communities who were required to receive services at a health facility. As part of the Coronavirus Preparedness and Response Supplemental Appropriations Act, Congress expanded the United States Department of Health and Human Services’ authority under Section 1135 of the Social Security Act to include waiver authority for certain Medicare telehealth restrictions during the pandemic. The Telehealth Extension and Evaluation Act would extend the telehealth expansions implemented under the 1135 waiver authority for two additional years at the end of the Public Health Emergency. MHA members with questions regarding the Telehealth Extension and evaluation Act should contact Laura Appel.
Rural Emergency Hospitals
In December 2020, Congress passed the Consolidated Appropriations Act (CAA) of 2021 (Public Law 116- 260), creating a new Medicare provider type called the Rural Emergency Hospital (REH). The REH will be a new rural hospital type that does not provide inpatient care but will provide 24-hour emergency services. By creating the REH, Congress has established the first new rural provider type in more than 20 years since the Critical Access Hospital (CAH) was created in 1997 under the Balanced Budget Act of 1997 (Public Law 105-33).
The legislation allows a CAH or small rural hospital with no more than 50 beds to convert to the REH provider type and begin providing services no earlier than Jan. 1, 2023. In preparation for this, the Department of Health & Human Services recently released the Rural Emergency Hospital Policy Brief and Recommendations to the Secretary. The brief includes 16 recommendations the Secretary of Health and Human Services should consider when finalizing the Rural Emergency Hospital’s program. Steve Barnett, CEO of McKenzie Health System, was a key contributing committee member. Special thanks to Steve for his contributions and ability to represent Michigan’s small and rural hospitals!
The Rural Health Information Hub recently held a webinar on the new REH designation. Members interested in learning more are encouraged to view the webinar slides.
The MHA has prepared a policy brief summarizing the current information that is available at the federal level on Rural Emergency Hospitals. Any hospital interested in exploring the REH designation should reach out to the MHA as soon as possible to express interest. Lauren LaPine currently sits on a state workgroup convened by the Michigan Department of Licensing and Regulatory Affairs to inform the licensure development process. Questions from member can be elevated to that workgroup, as appropriate.
The MHA has created several resources for hospitals pursuing the designation. Those resources include:
- Sample REH Talking Points.
- REH PowerPoint Presentation Template.
- REH Letter to the Board Template.
- REH Internal Newsletter Template.
- REH Op-ed Template.
Members considering the REH designation should reach out to Lauren LaPine.
CRNA
Legislation enhancing hospital flexibility for anesthesia care went into effect on Oct. 11, 2021. The MHA-supported legislation, House Bill 4359, was signed into law July 14 by Gov. Gretchen Whitmer. Sponsored by Rep. Mary Whiteford (R-Casco Township), the bill modernizes the scope of practice for certified registered nurse anesthetists (CRNAs) and allows flexibility for each hospital to choose the anesthesia care model that best fits its location, staffing and resources to offer safe and effective patient care by eliminating the state requirement that a CRNA must work under direct physician supervision.
Federal provisions have allowed states to request exemption from physician supervision of CRNAs under 42 CFR 482.852 upon passage of applicable laws and a letter of attestation from the governor to the Centers for Medicare & Medicaid Services. While this letter has not yet been sent, the MHA has requested that the governor perform this action and will keep members apprised of any official action. However, current federal provisions related to the COVID-19 pandemic and the federal Public Health Emergency allow CRNAs to practice without physician supervision without the further attestation of a letter from that state’s governor. Therefore, the provisions of HB 4359 are now in effect and allowed through at least the end of the federal public health emergency, which is currently in place and likely to continue through at least the end of the year.
The MHA worked with the Honigman Law Firm to develop additional resources for hospitals to assist with understanding the new law and the impacts of adopting new procedures. A memo outlines the details of the legislation, and a draft policy addendum provides additional information for members who need to amend their facility policies if they wish to use the flexibilities provided by the new law.
- Crain’s Detroit Business: New rule allows struggling rural hospitals to ditch non-emergency services
- Rural Innovation Exchange: Hospital CEOs: Time to retool rural health care is now
- Crain’s Detroit Business Op-Ed on Midsize Vital Hospitals
- Midsize Vital Hospital Infographic
- Critical Access Hospital Infographic
