Resources
Emergency Department Boarding for Behavioral Health Patients
Resources for Psychiatric Hospital Patients
Not All Wounds are Visible
On behalf of members, the MHA convenes a Behavioral Health Integration Council a minimum of four times per program year. Council members inform the policy and advocacy efforts that the MHA takes related to behavioral health issues in Michigan.
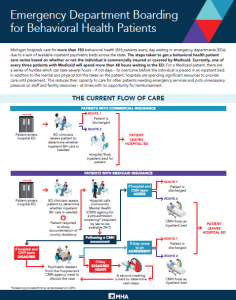
An infographic on the problems hospitals experience caring for behavioral health patients in the ED and proposed solutions will be shared with lawmakers. The resource includes data points from the MHA’s weekly behavioral health ED boarding survey.
Peer Recovery Coach Program Grant Recipients
The MHA awarded grant funding in June 2025 to seven Michigan healthcare organizations to support the development or expansion of hospital-based peer recovery coach (PRC) programs. The funding will support the addition of 18 new hospital-based PRCs and expand treatment options for patients with a substance use disorder.
The MHA received nine applications from organizations in seven distinct regions of the state, encompassing many innovative approaches to provide high-quality care for individuals experiencing substance use disorders.
These seven organizations, which were granted funding, are as follows:
- Aspire Rural Health System
- Bronson Healthcare
- Corewell Health East
- Henry Ford Health
- Memorial Healthcare
- Munson Healthcare
- Trinity Health Ann Arbor
Members with questions may contact Kelsey Ostergren at the MHA.
Resources for Psychiatric Hospital Patients
The MHA recently collaborated with the Mental Health Association of Michigan and Disability Rights Michigan to develop resources outlining patient rights in psychiatric hospitals across Michigan, Indiana, Wisconsin and Ohio. These assets are modeled after Disability Rights Ohio’s voluntary and involuntary patient rights materials in psychiatric hospitals.
These resources aim to help individuals, families and advocates understand key rights, including access to treatment, communication and safety. Whether an individual is a patient, caregiver or community advocate, these documents are designed to inform and empower.
Available in accessible formats such as PDF, Word and Large Print, these quick guides ensure equal access to critical rights information for people with disabilities, including those using screen readers or requiring larger text in psychiatric hospitals.
Statewide Assisted Outpatient Treatment Workgroup
The MHA participates in the Assisted Outpatient Treatment (AOT) Workgroup, which was created by Michigan’s Health Diversion Council. AOT is civil-court ordered community-based mental health treatment for those with serious mental illness that may include a period of hospitalization. AOT can be ordered anywhere in Michigan, but not every county has a comprehensive AOT program. Some counties do not have the need and/or capacity for an AOT program, and instead support individuals on AOT orders using available resources and services.
The Wayne State University Center for Behavioral Health and Justice, in partnership with the Michigan Department of Health and Human Services (MDHHS), developed an AOT toolkit for courts, community mental health agencies, jails and hospitals and health systems to use to expand statewide access to AOT. The MHA participates in this workgroup and represents hospitals and health systems who may encounter a patient with an order for AOT in the emergency department.
Members with questions regarding AOT should contact Lauren LaPine-Ray at the MHA.
Statewide Psychiatric Bed Registry
The MHA is collaborating with the MDHHS to create a statewide psychiatric bed registry in accordance with Public Act 658(8) of 2018. The law requires the State of Michigan to implement a statewide psychiatric bed registry, along with creating an advisory committee. As of Spring 2024, the intent is to create the statewide psychiatric bed registry within the EMResource platform. MHA hospitals and health systems will be kept appraised of changes and requirements that may result from the creation of the registry.
Members with questions on the statewide psychiatric bed registry should contact Lauren LaPine-Ray at the MHA.
Michigan Judicial Council Behavioral Health Improvements Workgroup
The MHA participates in the Michigan Judicial Council (MJC) Behavioral Health Improvements Workgroup to represent the interests of hospitals and health systems statewide. The workgroup was created based on as a result of the direction from the MJC’s strategic agenda and operational plan.
Chaired by Judge Michael Jaconette (Calhoun County Circuit Court and Mental Health Court), the workgroup develops new strategies to divert adults and youth with mental health and substance use disorders away from the justice system (criminal and civil) and connect them with needed behavioral health services instead. The workgroup studies the justice system’s response to behavioral health issues, makes recommendations for improvements across all case types and will issue a final report.
Members with questions on the MJC Behavioral Health Improvements Workgroup should contact Lauren LaPine-Ray at the MHA.
EMS Behavioral Health Transfer Workgroup
Convened by the MDHHS, the Emergency Medical Services Coordination Committee (EMSCC) is a multi-disciplinary group that works in an advisory capacity to the MDHHS, identifying barriers and recommending solutions about operationalizing emergency medical services (EMS) programs. The MHA and its members hold four seats on this committee.
The EMSCC Patient Movement Subcommittee is focused on identifying and addressing issues related to interfacility patient transport. One priority area for 2024 is improving interfacility transport of patients with acute behavioral health needs.
The MHA convened leadership from five behavioral health hospitals in April 2024 to share their perspective with the EMSCC subcommittee. This meeting was an initial step for both side to better understand the challenges they face and how the system can work more collaboratively to ensure safe and efficient transport of patients with behavioral needs.
Members with questions or requesting more information on the workgroup should contact Kelsey Ostergren at the MHA.
Psychiatric Residential Treatment Facilities
The MHA is working closely with the MDHHS to expand access to Psychiatric Residential Treatment Facilities (PRTF) statewide. The MDHHS aims to establish approximately 150 PRTF beds in the state. There are several key factors to consider if interested in establishing a PRTF:
- Does not require a Certificate of Need (CON).
- Contract is between the hospital and the MDHHS.
- Reimbursement rates negotiated directly with the MDHHS.
- Patients admitted to a PRTF may stay up to 180 days.
- Services to transition individuals out of a PRTF are identified/coordinated by the MDHHS directly.
The first step for hospitals or health systems interested in establishing a PRTF is to have a preliminary conversation with the MDHHS to learn more about the logistics.
Members interested in learning more about PRTFs should contact Lauren LaPine-Ray at the MHA.